Tip of the Month – November 2017: Multimodal Communication Therapy (MCT)
Multimodal Communication Therapy
Multimodal communication is all the different ‘modes’ that we communicate with, e.g. speaking face- to-face or over the phone, texting, writing, drawing, gesturing, acting it out, sign language, etc. Everyone, regardless of whether you have a communication difficulty or not, uses multiple modes to communicate each day.
People with aphasia can learn to use alternative forms of communication well during therapy sessions but often they do not generalise these skills to other environments. People with aphasia can learn to use a single modality (speaking or drawing or using a communication book) but they have trouble switching between modalities. Multimodal communication therapy* supports people with aphasia to learn to switch between the modalities in order to get their message across in lots of different ways. To encourage changing to a different modality to repair a communication breakdown, people with aphasia will learn many different modalities for a single concept rather than focusing on one specific modality at a time.
Often, people with aphasia will have a stronger or a weaker modality, e.g. they may get really ‘stuck’ when speaking, but they might be able to write the first few letters of the word. It is important to remember that aphasia can affect all aspects of language = speaking, understanding, reading and writing.
How to do multimodal communication therapy
This therapy session could be carried out by anyone (caregiver, spouse, daughter/son, etc under instruction by a Speech Therapist) and could be carried out a couple of times per day or only once per week. You could spent 10 minutes on each session or 30 minutes depending on motivation and fatigue.
- Write a list of 10-15 (or less if the person can’t cope with this many) words or phrases that the person with aphasia wants to practice. These should be motivating and functional. Start with words that can be easily drawn or acted out rather than abstract concepts. Family or caregivers might help the person with aphasia to select important words/phrases that they would like to practice. Then draw or print photos or pictures or write the words on large flash cards. E.g. cup of tea, watch Shortland Street, call Kelly, have you fed the dog, hungry, what time, etc.
- Choose at least three most functional modalities to practice, e.g. if writing and spelling is the most tricky modality then don’t practice this one because it will just cause frustration. Print out the modality prompt card, which you can use as a reminder of other modalities to try.
- Sit down in a quiet space and say “We are going to practice communicating these words/phrases in lots of different ways, so that when you get stuck, you can use a different way.”

- Hold up a picture or word from the list and say “how do you communicate this? Show me all the ways.”
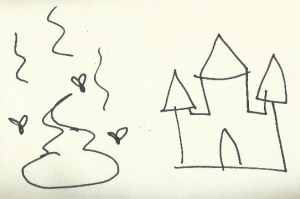
- The first time you need to model each of the modalities, e.g. you need to draw a picture of a cup of tea (you might want to use your non-dominant hand so that you are both learning to draw with a hand that is not used to holding a pen), and then get the person with aphasia to imitate you. Then gesture lifting a cup to your mouth and get the person with aphasia to imitate you. Then find 'cup of tea' in their communication book or device and so on.
- Make sure to give feedback to the person with aphasia when they do each modality – verbal directions of what they could do differently or hand over hand assistance may be needed.
- When you have practiced this list of words/phrases a few times (every day for a whole week or once per week for a month, etc) then make a new list. It might be useful to come back and revise previous lists from time to time.
- Hopefully you will start to see them using these different strategies in natural conversations. If they get stuck on a word or idea, remind them (with the prompt card) of the different modes they can use.
Here is a video of the difference that using or not using multiple modalities can make: https://www.youtube.com/watch?v=KWVoqM9jmEM
Resources
You don’t need ‘special’ apps or devices or therapy ‘programmes’ to use multimodal communication.
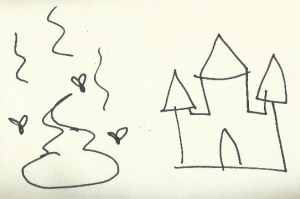
- Pen and paper – it is helpful to have a blank book that the person with aphasia can carry around and do all new drawings or writing in that book because they might want to refer back to things they have previously drawn or written during new conversations. This is also helpful for communication partner to write choices for the person with aphasia to choose from or to write down key words to clarify the topic of conversation and what the message is.
- Whiteboard and marker – this is helpful for ‘on the go’ conversations and you can always take a photo of the whiteboard if you talk about important topics and want a record to look back at later.
- Maps – these can be helpful in providing context.
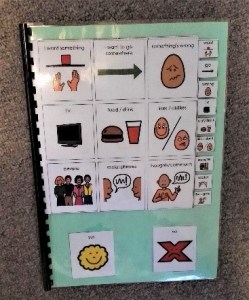
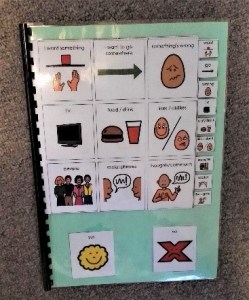
- Communication book or device – this can be a single paper, a full book of vocabulary or a speech generating device.
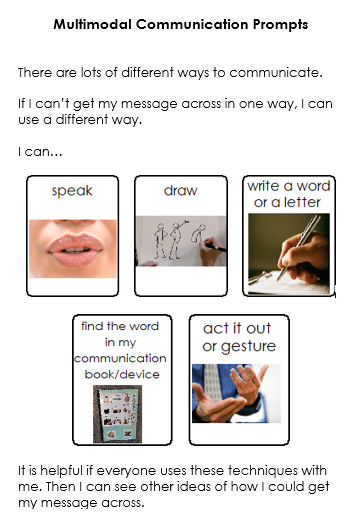
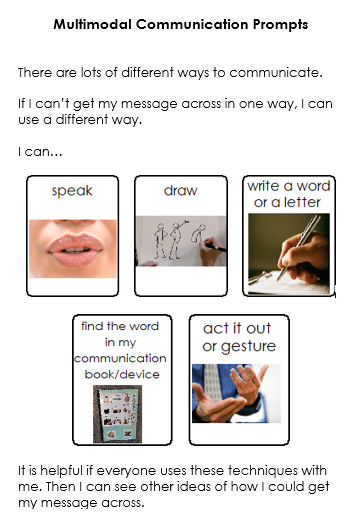
- Prompt sheet – a prompt sheet (like the examples below) can be helpful in reminding everyone who is communicating that there are lots of different ways to communicate and if one mode does not work, there are other options to try. You could print this out and stick it in the book for drawing/writing book OR as a small “business card” in their wallet.
Extras
Here are some good reminders for communicating with adults with aphasia: https://www.youtube.com/watch?v=FWOYmqyDooc
References:
Mikola, J. (2011). Communication competence in persons with aphasia: The impact of executive functions. Dissertation Abstracts International: Section B: The Sciences and Engineering (7-B), 4215.
Nicholas, M., Sinotte, M., & Helm-Estabrooks, N. (2011). C-Speak Aphasia alternative communication program for people with severe aphasia: importance of executive functioning and semantic knowledge. Neuropsychological Rehabilitation, 21, 322-366.
Purdy, M., Duffy, R.J., & Coelho, C.A. (1994). An investigation of the communicative use of trained symbols following multimodality training. Clinical Aphasiology, 22, 345-356.
Purdy, M. (2002). Executive functioning in aphasia. Aphasiology, 16, 549-557.
Purdy, M. & Wallace, S.E. (2016). Intensive multimodal intervention for severe aphasia. Aphasiology, 30, 1071-1093.
Wallace, S. E., Purdy, M., & Skidmore, E. (2014). A multimodal communication program for aphasia during inpatient rehabilitation: A case study. Neurorehabilitation, 35, 615-625
Wallace, S.E., & Diehl, S. (2017). Multimodal Communication Program for adults: Cognitive considerations. Perspectives of the ASHA Special Interest Groups, SIG 12(2), 4-12.
Wallace, S.E. & Purdy, M. (2013). More than words. The ASHA Leader
Yoshihata, H., Watamori, T., Chujo, T., & Masuyama, K. (1998). Acquisition and generalization of mode interchange skills in people with severe aphasia. Aphasiology, 12, 1035-1045.
Multimodal Communication Therapy
Multimodal communication is all the different ‘modes’ that we communicate with, e.g. speaking face- to-face or over the phone, texting, writing, drawing, gesturing, acting it out, sign language, etc. Everyone, regardless of whether you have a communication difficulty or not, uses multiple modes to communicate each day.
People with aphasia can learn to use alternative forms of communication well during therapy sessions but often they do not generalise these skills to other environments. People with aphasia can learn to use a single modality (speaking or drawing or using a communication book) but they have trouble switching between modalities. Multimodal communication therapy* supports people with aphasia to learn to switch between the modalities in order to get their message across in lots of different ways. To encourage changing to a different modality to repair a communication breakdown, people with aphasia will learn many different modalities for a single concept rather than focusing on one specific modality at a time.
Often, people with aphasia will have a stronger or a weaker modality, e.g. they may get really ‘stuck’ when speaking, but they might be able to write the first few letters of the word. It is important to remember that aphasia can affect all aspects of language = speaking, understanding, reading and writing.
How to do multimodal communication therapy
This therapy session could be carried out by anyone (caregiver, spouse, daughter/son, etc under instruction by a Speech Therapist) and could be carried out a couple of times per day or only once per week. You could spent 10 minutes on each session or 30 minutes depending on motivation and fatigue.
- Write a list of 10-15 (or less if the person can’t cope with this many) words or phrases that the person with aphasia wants to practice. These should be motivating and functional. Start with words that can be easily drawn or acted out rather than abstract concepts. Family or caregivers might help the person with aphasia to select important words/phrases that they would like to practice. Then draw or print photos or pictures or write the words on large flash cards. E.g. cup of tea, watch Shortland Street, call Kelly, have you fed the dog, hungry, what time, etc.
- Choose at least three most functional modalities to practice, e.g. if writing and spelling is the most tricky modality then don’t practice this one because it will just cause frustration. Print out the modality prompt card, which you can use as a reminder of other modalities to try.
- Sit down in a quiet space and say “We are going to practice communicating these words/phrases in lots of different ways, so that when you get stuck, you can use a different way.”

- Hold up a picture or word from the list and say “how do you communicate this? Show me all the ways.”
- The first time you need to model each of the modalities, e.g. you need to draw a picture of a cup of tea (you might want to use your non-dominant hand so that you are both learning to draw with a hand that is not used to holding a pen), and then get the person with aphasia to imitate you. Then gesture lifting a cup to your mouth and get the person with aphasia to imitate you. Then find 'cup of tea' in their communication book or device and so on.
- Make sure to give feedback to the person with aphasia when they do each modality – verbal directions of what they could do differently or hand over hand assistance may be needed.
- When you have practiced this list of words/phrases a few times (every day for a whole week or once per week for a month, etc) then make a new list. It might be useful to come back and revise previous lists from time to time.
- Hopefully you will start to see them using these different strategies in natural conversations. If they get stuck on a word or idea, remind them (with the prompt card) of the different modes they can use.
Here is a video of the difference that using or not using multiple modalities can make: https://www.youtube.com/watch?v=KWVoqM9jmEM
Resources
You don’t need ‘special’ apps or devices or therapy ‘programmes’ to use multimodal communication.
- Pen and paper – it is helpful to have a blank book that the person with aphasia can carry around and do all new drawings or writing in that book because they might want to refer back to things they have previously drawn or written during new conversations. This is also helpful for communication partner to write choices for the person with aphasia to choose from or to write down key words to clarify the topic of conversation and what the message is.
- Whiteboard and marker – this is helpful for ‘on the go’ conversations and you can always take a photo of the whiteboard if you talk about important topics and want a record to look back at later.
- Maps – these can be helpful in providing context.
- Communication book or device – this can be a single paper, a full book of vocabulary or a speech generating device.
- Prompt sheet – a prompt sheet (like the examples below) can be helpful in reminding everyone who is communicating that there are lots of different ways to communicate and if one mode does not work, there are other options to try. You could print this out and stick it in the book for drawing/writing book OR as a small “business card” in their wallet.
Extras
Here are some good reminders for communicating with adults with aphasia: https://www.youtube.com/watch?v=FWOYmqyDooc
References:
Mikola, J. (2011). Communication competence in persons with aphasia: The impact of executive functions. Dissertation Abstracts International: Section B: The Sciences and Engineering (7-B), 4215.
Nicholas, M., Sinotte, M., & Helm-Estabrooks, N. (2011). C-Speak Aphasia alternative communication program for people with severe aphasia: importance of executive functioning and semantic knowledge. Neuropsychological Rehabilitation, 21, 322-366.
Purdy, M., Duffy, R.J., & Coelho, C.A. (1994). An investigation of the communicative use of trained symbols following multimodality training. Clinical Aphasiology, 22, 345-356.
Purdy, M. (2002). Executive functioning in aphasia. Aphasiology, 16, 549-557.
Purdy, M. & Wallace, S.E. (2016). Intensive multimodal intervention for severe aphasia. Aphasiology, 30, 1071-1093.
Wallace, S. E., Purdy, M., & Skidmore, E. (2014). A multimodal communication program for aphasia during inpatient rehabilitation: A case study. Neurorehabilitation, 35, 615-625
Wallace, S.E., & Diehl, S. (2017). Multimodal Communication Program for adults: Cognitive considerations. Perspectives of the ASHA Special Interest Groups, SIG 12(2), 4-12.
Wallace, S.E. & Purdy, M. (2013). More than words. The ASHA Leader
Yoshihata, H., Watamori, T., Chujo, T., & Masuyama, K. (1998). Acquisition and generalization of mode interchange skills in people with severe aphasia. Aphasiology, 12, 1035-1045.
